One of our goals at VTLyme.com is to ensure Vermonters have accurate information about Lyme and tick-borne diseases specific to Vermont. This review of local media reports, newspapers, and newsletters shows that even among medical and science professionals there is confusion about the diagnosis and treatment of Lyme disease in Vermont. In addition, only two articles mentioned the presence of other tick-borne diseases in Vermont, such as Anaplasmosis.
Vermonters have a right to accurate and unbiased information about Lyme and tick-borne diseases so they can make informed decisions about their health care. Medical professionals in Vermont should be aware of the varied presentations of Lyme disease, and the limitations of blood tests, so Vermont patients can have access to effective diagnosis and treatment. Institutions, such as the Vermont Department of Health, should be working to ensure that accurate and thorough information about Lyme disease in Vermont is available to journalists, health professionals, and all Vermonters.
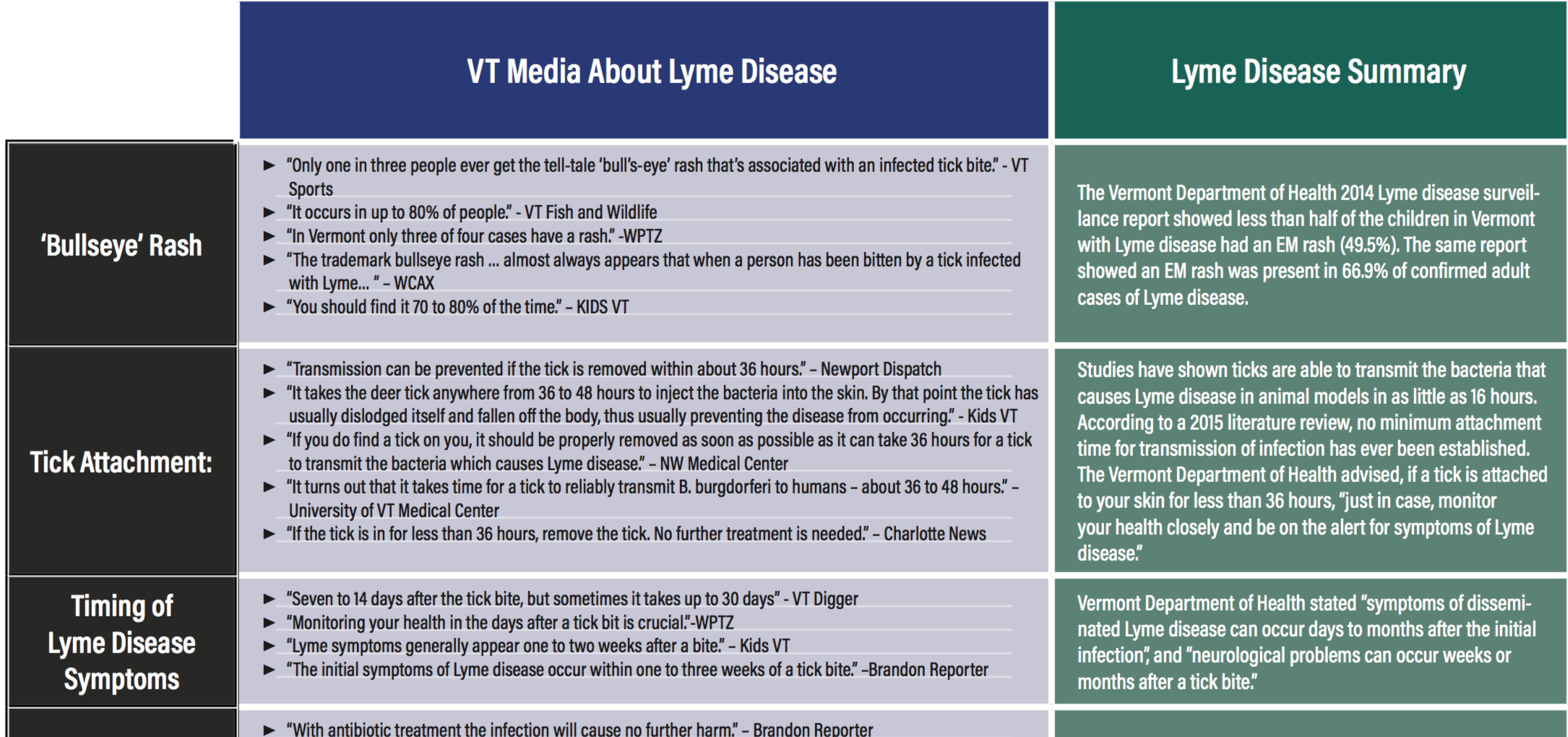
An informal analysis of Vermont newspaper, newsletters, and media reports about Lyme disease from 2014-2016 revealed contradicting and inaccurate statements about Lyme disease symptoms, diagnosis, and treatment. Some examples are listed below:
| VT Media About Lyme Disease | Lyme Disease Summary | |
|---|---|---|
| ‘Bullseye’ Rash |
|
The Vermont Department of Health 2014 Lyme disease surveillance report showed less than half of the children in Vermont with Lyme disease had an EM rash (49.5%). The same report showed an EM rash was present in 66.9% of confirmed adult cases of Lyme disease. |
| Tick Attachment: |
|
Studies have shown ticks are able to transmit the bacteria that causes Lyme disease in animal models in as little as 16 hours. According to a 2015 literature review, no minimum attachment time for transmission of infection has ever been established. The Vermont Department of Health advised, if a tick is attached to your skin for less than 36 hours, “just in case, monitor your health closely and be on the alert for symptoms of Lyme disease.” |
| Timing of Lyme Disease Symptoms |
|
Vermont Department of Health stated “symptoms of disseminated Lyme disease can occur days to months after the initial infection”, and “neurological problems can occur weeks or months after a tick bite.” |
| Treatment for Lyme Disease |
|
Approximately 10-20% of people treated for Lyme disease have continuing symptoms a year after treatment. Some individuals have been disabled by Lyme. The earlier a person is diagnosed with Lyme disease, the more likely standard treatment will work. Most people recover fully from Lyme disease when it is promptly diagnosed and appropriately treated. |
| Diagnosis of Lyme Disease |
|
According to the CDC Lyme disease is “diagnosed based on symptoms, physical findings and the possibility of exposure to infected ticks.” A negative blood test does not mean you do not have Lyme disease. False negatives and false positives do occur. |
Click here for the Printable Misinformation Clarification Chart [PDF]